Somewhere right now, a doctor is finishing charting at 10:47pm, staring at a stack of claims that “just need to be checked and sent.” Everyone says they got into medicine to help people. No one ever says, “I became a physician for the joy of CPT codes and payer portals.”
And yet, here we are.
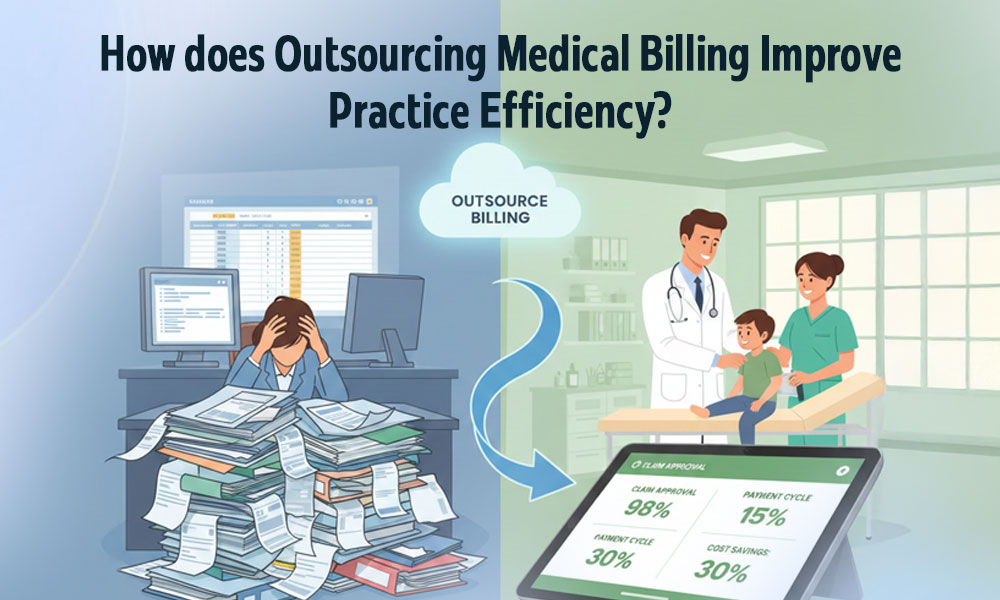
That’s why medical outsourcing exists. Not as some trendy buzzword, but as the quiet admission that your clinic is pretending to be a billing company on the side…and doing a pretty average job of it.
When you move to outsourced medical billing, you’re not “losing control.” You’re admitting that other humans wake up excited to think about denial codes, fee schedules, and CMS updates, and maybe, just maybe, you should let them.
Here’s how outsourcing medical billing doesn’t just save money: it makes your whole practice breathe easier and move faster.
1. Doctors Go Back to Being Doctors (Instead of Surprised Clerks)
- In‑house billing steals time.
Staff split between phones, front desk, and claims. Clinicians get dragged into coding disputes, prior auth drama, and “why was this denied?” autopsies.
- Medical billing services flip the script.
Front desk focuses on patients. Clinicians focus on care. The billing team -external and specialized – handles the weird payer stuff full time.
- Result:
More face‑to‑face minutes with patients. Less brain space spent on admin. Better outcomes, fewer burnout fantasies about quitting to run a bookstore.
2. Operational Costs Stop Feeling Like a Leaky Faucet

- In‑house billing = salaries + benefits + office space + training + software + turnover.
Every time a biller quits, you restart the entire expensive cycle.
- With outsourced medical billing:
You pay a percentage of collections or a clear fee. No payroll taxes. No sick leave. No “we need $8k for another billing software upgrade.”
- Efficiency:
Practices routinely cut billing‑related operational costs by 20–30% when they move to external teams that already have tools, training, and processes dialed in.
3. Cash Flow Speeds Up Instead of Limping Along
- Slow claims = slow paychecks.
Late submissions, incomplete info, weak follow‑up—your AR grows a nice grey beard.
- Medical billing experts live in the revenue cycle.
They push clean claims out fast, track them, and chase payers instead of shrugging and saying, “We’ll resubmit later.”
- What changes:
- Fewer rejections → fewer resubmissions.
- Faster appeals on denials.
- Regular follow‑ups instead of “maybe next week.”
- Outcome:
Practices see cash flow improve noticeably – money shows up in weeks, not months. Payroll becomes less of a nail‑biter.
- Billing Errors Drop, Denials Follow
- In‑house teams juggle a thousand things.
One missed modifier, one wrong code, one outdated rule—and your claim goes into the payer’s trash bin.
- A medical biller specialist breathes this work.
Up‑to‑date codes, payer rules, documentation requirements. Accuracy is not “nice to have”; it’s survival.
- Fewer errors =
- Fewer denials.
- Less time fixing, rebilling, re‑waiting.
- Less money silently evaporating.
- Translation:
You stop paying to do the same work twice.
5. Compliance Stops Being a Guessing Game
- Regulations change like weather: Medicare updates, payer policy changes, state rules.
Missing something can cost you—audits, fines, clawbacks, lovely letters with lots of legal words.
- Medical billing experts track this for a living.
HIPAA, CMS, payer bulletins—someone on their side is always reading that stuff so you don’t have to.
- Efficiency gain:
You don’t lose weeks reacting to new rules. Your process quietly adapts, and claims keep moving.
6. You Get a Whole Team, Not Just One Overwhelmed Person
- One in‑house biller = single point of failure.
They get sick, take leave, or ‘quit—billing ‘stops or falls to whoever looks most unlucky.
- Medical outsourcing gives you a team:
Coders, follow‑up staff, denial specialists, credentialing people, all under one roof.
- Benefits:
- Work continues if one person is out.
- Different brains for different problems.
- More built‑in quality checks.
- Net effect:
Your revenue cycle stops depending on one person’s emotional state and vacation schedule.
7. Your Practice Actually Scales Without Breaking
- Growth usually looks like: more patients → more chaos → more staff → bigger payroll → same chaos with better chairs.
- With outsourced medical billing:
You can add providers or locations without rebuilding your internal billing department every time.
- Scalability:
- Volume up? Vendor adds capacity.
- Volume down? You don’t carry idle billers on payroll.
- This is how practices move from “we’re busy” to “we’re growing on purpose.”
8. Patients Get Fewer Confusing Bills (and Complain Less)
- Sloppy billing = confused patients.
Wrong codes, late statements, double charges → angry calls, negative reviews, people switching providers over money drama.
- Solid medical billing services:
- Generate clear, timely statements.
- Fix mistakes faster.
- Communicate better about balances and insurance breakdowns.
- Efficiency isn’t just internal.
Happier patients call less, argue less, pay faster, and stay longer.
9. Billing Turns from a Cost Center into a Revenue Engine
- Before:
Billing feels like overhead. Something you pay for just to not drown.
- After outsourcing to real medical billing experts:
- Under‑coded visits get corrected.
- Missed charges get caught.
- Denials get appealed instead of forgotten.
- Suddenly:
The same patient volume generates more collected revenue. Not because you’re charging more, but because you’re collecting what you should have been all along.
10. You Get Visibility Instead of Vibes
- Most practices “feel” how they’re doing.
Busy waiting room? Must be good. Empty? Must be bad. That’s not data. That’s vibes.
- External billing teams often provide:
- Monthly performance reports
- Denial breakdowns
- Payer mix insights
- Collection timelines
- With that:
You can make decisions – about contracts, staff, services – with actual numbers in front of you.
Efficiency here means fewer blind guesses and fewer “we’ll just see how next quarter goes.”
Where Remote Resource Fits Into This Circus
You can try to navigate the medical outsourcing world alone…interviewing vendors, reading proposals, deciphering percentages, and hoping “we’re very experienced” means something.
Or you can let someone who lives in this space do the heavy lifting.
Remote Resource helps practices:
- Find medical billing experts who fit your specialty and size.
- Avoid vendors who talk pretty and perform poorly.
- Set up outsourced medical billing without breaking your staff (or your sanity) in the transition.
Instead of turning your clinic into a full‑time billing experiment, you get a shorter route: people who know what good looks like, and how to plug it in.
Medical Outsourcing Challenges in 2026 & Beyond
1. The Fear of Losing Control (And Sometimes Actually Losing It)
- Handing billing to an outside team feels like handing your wallet to a stranger with a nice smile.
- If you don’t set clear rules – who decides what, who sees what, how often you review reports- you can wake up feeling like a passenger in your own practice.
What it looks like in real life:
- You don’t know which claims are pending.
- You see deposits but not patterns.
- Leadership meetings turn into “we think they’re doing fine.”
Control isn’t lost by outsourcing. It’s lost by not demanding transparency and regular check‑ins.
2. Communication Gaps Across Time Zones and Time Pressure
- Your clinic runs on “right now.”
- Billing vendors often run on “next batch, tomorrow.”
Common friction points:
- Slow responses on urgent denials.
- Delays in clarifying missing documentation.
- Time zone mismatch where your morning crisis is their 2am.
If you don’t agree on response times, escalation paths, and communication channels up front, the efficiency you gain on claims can get eaten by frustration and back‑and‑forth emails.
3. One‑Size‑Fits‑Nobody Processes
- Some medical billing services operate like factories: one template for everyone.
- Your practice has quirks…visit patterns, payer mix, specialties, local rules.
The clash:
- Their scripts don’t match how your front desk collects info.
- Their coding assumptions don’t match your clinical reality.
- Their reports don’t answer your questions.
You save time on execution but lose nuance in how your particular practice actually makes money.
4. Data Security and Trust Issues
- You’re sending PHI out the door—claims, demographics, clinical notes.
- That’s not a small thing in a world of breaches and ransomware.
Real worries:
- Weak internal controls at the vendor.
- Third‑party subcontractors you never met touching your data.
- No real plan if something goes wrong beyond “we’re sorry.”
In 2026, every extra system and every extra human in the chain is another possible leak. Outsourcing means your risk shifts – you don’t escape it.
5. Vendor Lock‑In and the “We Can’t Leave” Problem
- At first, you outsource to get relief.
- Three years later, all your processes, payer contacts, and billing history effectively live in their world.
Then:
- Switching vendors looks terrifying.
- Bringing billing back in‑house looks impossible.
- You feel you’re negotiating from a weaker position.
If contracts, data exports, and knowledge transfer aren’t sorted early, “outsourced medical billing” can start to feel like a very polite trap.
The Bottom Line
If your days are full, your staff is fried, and your cash flow never quite feels as healthy as your patient list, it’s probably not your medicine. It’s your billing pretending to be a side hobby.
Outsource the thing that’s slowing you down. Let people who love codes and claims do codes and claims.
Remote Resource can connect you with the medical billing experts who turn revenue chaos into something predictable, calm, and surprisingly profitable!